Pandemic dilemmas for UK policy makers
Since my last post on the subject of modelling the UK pandemic, quite a few things have changed.
In the real world, we’ve all become experts on virus variants and quite a lot of research has been published on the effectiveness of the vaccines and other key modelling assumptions. We also have four more weeks of data on case numbers and how they are responding to the lockdown.
For myself, I’ve done quite a bit of development on my model. Previously, I was only dividing the population into two age groups, the over 70s and the rest. Now I have 10 age bands. I’ve also added the ability to deal with multiple variants and model the impact of differing levels of infectiousness and vaccine effectiveness.
With the UK government due to set out its plans for the “gradual and phased” route out of lockdown in just over a week, I thought people might be interested to see what my new and improved model says about the policy options and what they might mean for how things could unfold over the next few months.
I’ll start with the assumptions for vaccine effectiveness, including the important issue of whether vaccines will reduce spread as well as providing personal protection against disease.
Vaccine effectiveness
I have been using an assumption for vaccine effectiveness of 70% after the first dose and 80% after the second. In my model, this parameter determines the likelihood of becoming infected. It also drives the risk of getting symptoms, being hospitalised, dying and spreading the virus to others. In the real world, vaccines affect each of these risks differently.
In truth, very little solid evidence of the impact of vaccines on transmission has been available until recently. The vaccine efficacy figures that were published initially were about the reduced risk of getting a symptomatic case of the disease. Nobody really knew to what extent the vaccines just turned symptomatic infections into asymptomatic ones, with people still just as likely to catch and pass on the virus.
A paper has now been published which addresses this question for the Oxford - Astra Zeneca shot, the main vaccine being used in the UK. It estimates that the first dose reduces the chances of becoming infected by 67%. That’s not quite the same thing as transmission, since that also depends on whether the 33% that do become infected have the same propensity to spread the disease as an unvaccinated person. This could go either way. More of the infections will be asymptomatic, which might increase onward spread. People who have no symptoms and have the added feeling of safety from having been vaccinated might be less cautious. On the other hand, we know that vaccines lead to milder cases, presumably due to reduced viral load. That may reduce spread. In the absence of further data to judge, I’ve made what I hope is a neutral assumption that first dose vaccination reduces transmission by 67%.
The same paper says that the vaccine provides protection against developing a symptomatic infection of 76% after one dose and 82% after two, slightly higher than the assumptions I had been using, so I’ve adjusted my assumptions accordingly.
The final question is what impact the second dose vaccination has on transmission. I’ve assumed that there is a similar increase as we see for protection against symptoms and so I’ve used 72%. That is lower than what has been found for the level of protection against reinfection provided by natural immunity of 83%.
Vaccine impact on hospitalisations and deaths
All of the research findings that have been published so far have found no hospitalisations or deaths amongst people who have received both doses. That seems to suggest a 100% protection factor against serious disease.
But we need to remember that we are talking about very small numbers of cases here. For example, in the Astra Zeneca study, there were 6 hospitalisations amongst the 12,104 people in the control group and none in the 12,408 vaccinated group. Even just allowing for the 67%+ reduction in infection rate would reduce the expected number of hospitalisations amongst the vaccinated group to 2 or fewer cases.
I’ve decided to assume that the vaccines provide 79% protection against getting hospitalised or dying after one dose and 90% after two. Hopefully, that will prove to be a cautious assumption and the levels of protection will actually be higher.
Variants
In my previous modelling work, I only allowed for a single version of the virus, which I took to be the new “Kent” variant (also known as B.1.1.7). I assumed it was just over 50% more transmissible than the original strain. There have been papers published which cast doubt on whether the increase in transmissibility is as high as this, such as this one, which estimates the increase at only 25%. After doing some back testing of my model, I am inclined to think that 50% is too high. Simply put, the Kent variant now represents about 90% of cases in the UK, and cases have been falling faster than might be expected if its transmissibility was really 50% higher. So I’ve reduced my assumption to 35%.
The government has suggested that there are some “hints in the data” that the Kent variant also has a higher mortality rate. Scientists have pushed back on this, citing the lack of any real evidence, and as a result I have not made any allowance for this.
We have good evidence that the current vaccines work as well against the Kent variant as they do against the original strain. But the same is not the case for the “South Africa” strain or other variants with the E484K mutation
Initial results have been published on the effectiveness of the as yet unapproved Janssen vaccine, which was extensively tested in both the USA and in South Africa. These suggest that its effectiveness against the South Africa variant is 15 points lower than against the original strain prevalent in the US. Nobody really knows whether those results will apply equally to the Oxford - Astra Zeneca or to other vaccines, but for the purposes of my modelling work, that is what I have assumed. So instead of reducing infection risk by 67% after one dose, I assume 52% for the South Africa variant.
Vaccine rollout and take-up
I’ve assumed that the vaccine rollout continues at the current pace. In my base case, I’ve estimated take-up from the under 60s at 85% and eligibility restricted to those aged 18 and over. That sees all eligible people being offered a vaccination by early July, with the last second doses delivered twelve weeks later.
As we will see in a moment, that doesn’t seem to be enough to achieve herd immunity. It may be the case that uptake will be better than 85%, but the bigger difference would come from vaccinating under 18s. There are 9.5 million people aged 6 to 17, representing 14% of the population. Vaccinating 85% of those would add 8.0m people with immunity compared to the 3.7m extra you would get from increasing takeup amongst the 18 to 59 year olds to 95%.
Currently the vaccines are only authorised in the UK for those 18 years or older, but the Pfizer vaccine is already authorised for 16 year olds in the US and a trial of the Oxford Astra Zeneca vaccine on 6 to 17-year olds is about to begin in the UK . So I’ve explored a scenario where children aged 6 years or more also get vaccinated.
Options to relax the lockdown
I assume that the current restrictions are suppressing spread by 70%. I’ve taken as a base case that the government will choose to reopen schools on the 8th March, which reduces suppression to 60%. That is followed by a further relaxation at the start of May to 40% suppression, which I think is around the levels that the UK had in the summer last year. A final relaxation to 20% suppression is then enacted at the end of July, representing a return to “normal life”, but with some on-going changes to behaviour.
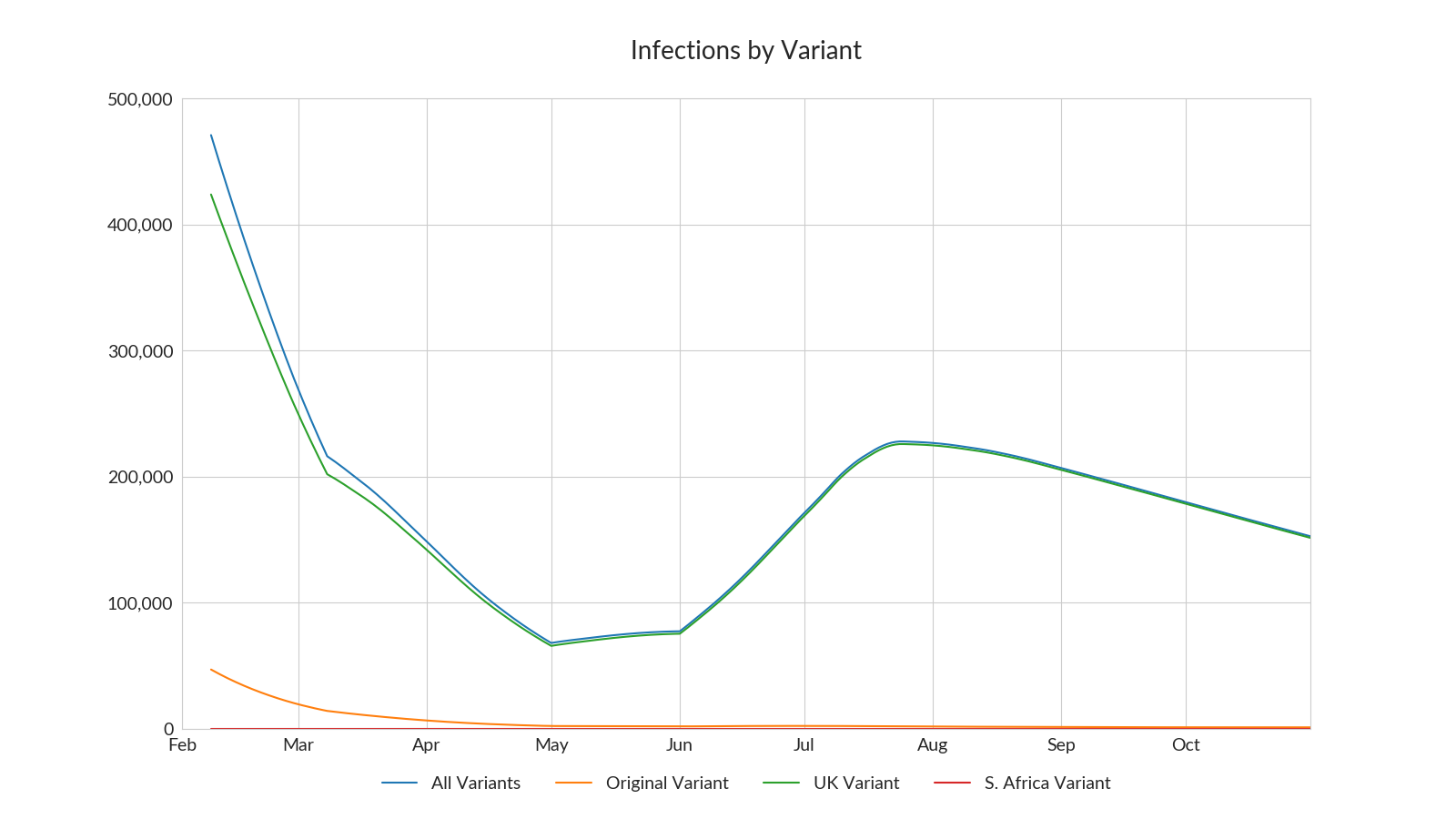
The following chart shows how infectious cases develop under this scenario, assuming the South Africa variant never gets established. The relaxation in May does cause cases to begin to rise again, but they are quickly brought back under control as the vaccination programme continues to roll out.
As mentioned earlier, cases do begin to grow again following the final relaxation of restrictions in August, showing that under the base case assumptions, herd immunity is not reached and cases will begin to grow again if restrictions are fully relaxed.
However, vaccinating children 6 years or older fixes this, as we can see from the following chart where I show the projections if I make that assumption.
What about new variants?
Currently, only 170 confirmed cases of the South Africa variant have been identified in the UK. Even if the real number is 10 times that, that would still only represent about 0.3% of cases and the government is trying really hard to prevent community spread and avoid new cases being imported from overseas travel.
You can see why they are so keen to do this from considering the following scenario, where I’ve added South Africa variants at 0.3% of cases at the start of the simulation.
As long as restrictions are in place, the South Africa variant doesn’t take off. It is no more infectious than the UK variant and restrictions contain the spread of both strains. But as restrictions are relaxed and more of the burden of containing spread comes to rely on population immunity, it begins to grow faster than the UK variant. If restrictions are fully relaxed at the start of August, infections will begin to take off again.
New versions of the vaccines are under development and should be ready for deployment in the Autumn. But giving booster shots will take time, so you can see why the government is keen to delay the arrival of the new variants.
What about the “Big Wave” option?
There is of course another strategy that the government could pursue. Once older and other higher risk people have all been offered the vaccine, restrictions could be relaxed at a much faster rate. Even though that would result in a big wave of infections, the vaccines should prevent hospitalisation numbers becoming unmanagable and significantly reduce the likely additional number of deaths.
Some have been proposing that once the over 50s and other higher risk people have been vaccinated, restrictions should be relaxed, regardless of the implications for case numbers.
The following chart shows my projection for the percentage of each age band that will have received both doses over time. My prediction is that the over 50s should be done by the end of May.
So, in my first “Big Wave” scenario, I’ve assumed a full relaxation from the start of June. This projection is based on the South Africa variant not becoming established and children getting vaccinated. So the best case assumptions for the Big Wave proponents.
As you might expect, cases do indeed start to rise again, but due to the increasing immunity provided by the vaccination programme, this is not a particularly big wave compared to the one we are in at the moment.
Hospitalisations also rise again, but the additional protection provided by the vaccines mean that hospital cases reach nothing like the current levels. So there is no argument against this option based on the need to “protect the NHS”. In the chart below I’ve included the data for recent history to provide context.
In terms of other metrics, there are 3,400 more deaths in this scenario compared to the base case. Cumulative cases would be 1.9 million higher, so an extra 3% or so of the population would get infected, but almost all would be mild or asymptomatic cases.
So this does appear to be a very valid option.
A proper Big Wave scenario
Big Wave proponents may argue that waiting until June is still being too cautious. Let’s look at an even more aggressive relaxation, where all restrictions are dropped from the start of April. That’s about two weeks after the over-50s should have received their first dose.
This gives a properly big wave of infections, peaking at almost 2 million cases towards the end of June.
Once again, the protection provided by the vaccines for the higher risk groups against hospitalisation makes this option doable from a health care capacity point of view, as the following chart shows.
The main issue with this scenario would be the number of deaths, which I think would be about 30,000 higher than in the base case. If that forecast is accurate, I would imagine that is too high a price to accept politically, in exchange for the benefit of opening things up two months earlier.
Conclusions
My first conclusion is that if the UK can buy at least a couple of months without the South African variant starting to spread, the modified vaccines should arrive in time to be able to deal with it, if and when it does arrive.
Secondly, as long as the assumptions about the efficacy of the vaccines hold up and the vaccination programme continues to proceed as planned, the need to avoid overwhelming the health care system should cease to be a hard constraint from the start of April, or possibly even earlier.
From that time onwards, there should be a considerable degree of choice for policy makers, depending on priorities. My own guess is that a middle road will be taken, with restrictions progressively relaxed during April and May and life back to something quite close to normal by the summer.
Of course the big question for the travel industry is whether that includes the freedom to travel overseas. I think that you could make a credible case for either approach based on the science - there is still quite a bit of uncertainty about key assumptions. Further data will become available over the next couple of months which may help inform policy decisions, but in the end this will inevitably be driven by the political pressures, once the science is not decisive.
At the moment, overseas travel is viewed as something to be outlawed and eliminated and travel restrictions enjoy broad public support. But as case numbers drop, hospitals empty and people get their vaccinations, I think it is likely that the balance of public opinion will rapidly begin to shift. If that happens, politicians will surely follow the votes rather than the more cautious voices amongst the scientists.
However bleak the outlook for the UK travel industry seems to be at the moment, perhaps the old saying about it always being darkest before the dawn will prove to be true.